The Response of Provincial Health Systems to COVID-19: Service Provision and Costs Across Health Sectors, First Nations and other populations.
Principal Investigators: Krahn M, Kulkarni G
Co-Investigators: Cheung D, Del Giudice L Finelli A, Hillmer M, Lapointe-Shaw L, McGrail K, Mendlowitz A, Peacock S, Perlis N, Rabeneck L, Tomlinson G, Walker J, Wong W
Click HERE for official CIHR Funding Notification details.
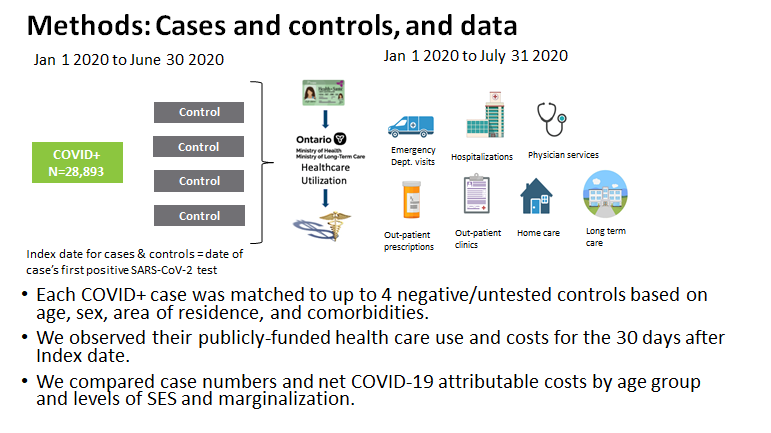
A team of researchers is focusing on the effects of COVID19 on individuals not diagnosed with coronavirus including those living in remote regions of British Columbia and Ontario, and First Nations peoples. Professors Murray Krahn and Girish Kulkarni are leading the study, The Response of Provincial Health Systems to COVID-19: Service Provision and Costs Across Health Sectors, First Nations and other populations. They will also examine costs and resource use by COVID-19 patients.
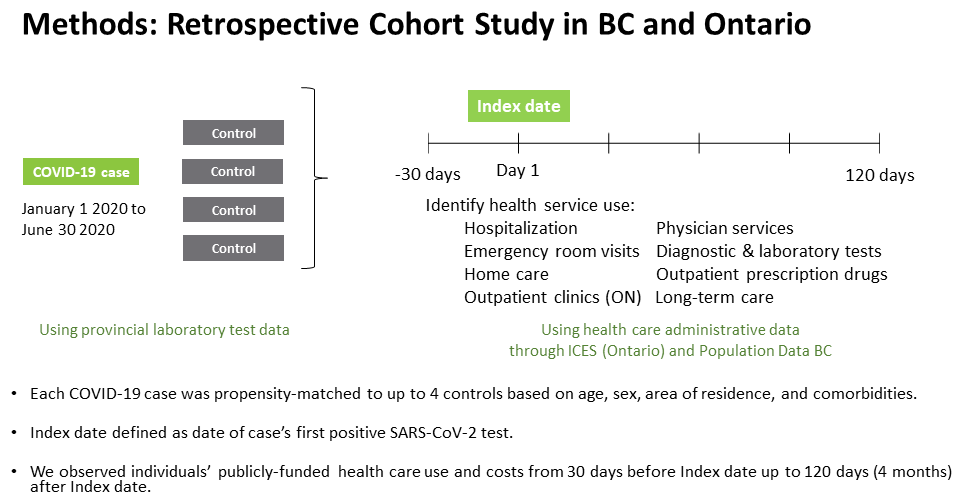
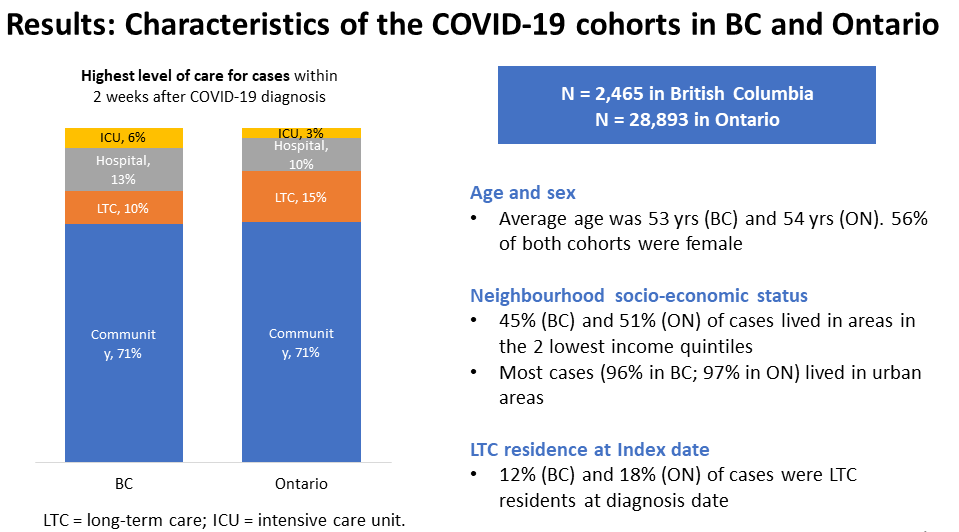
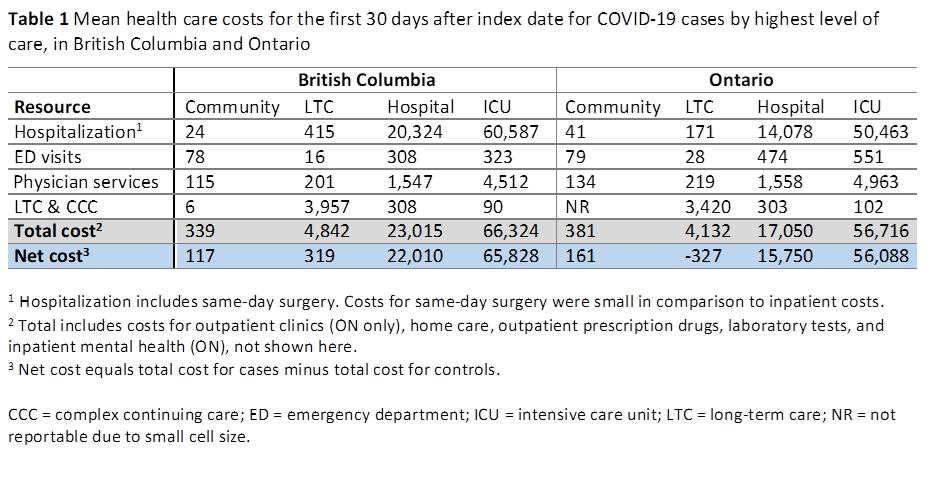
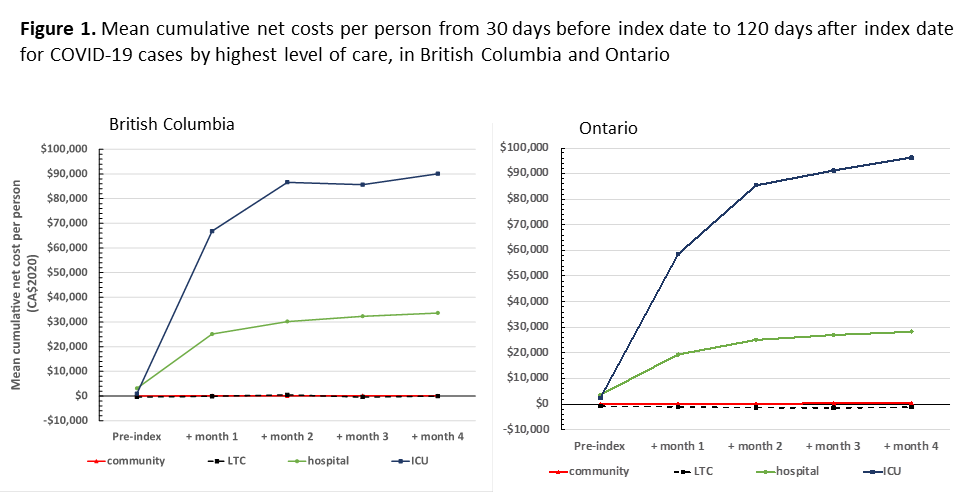
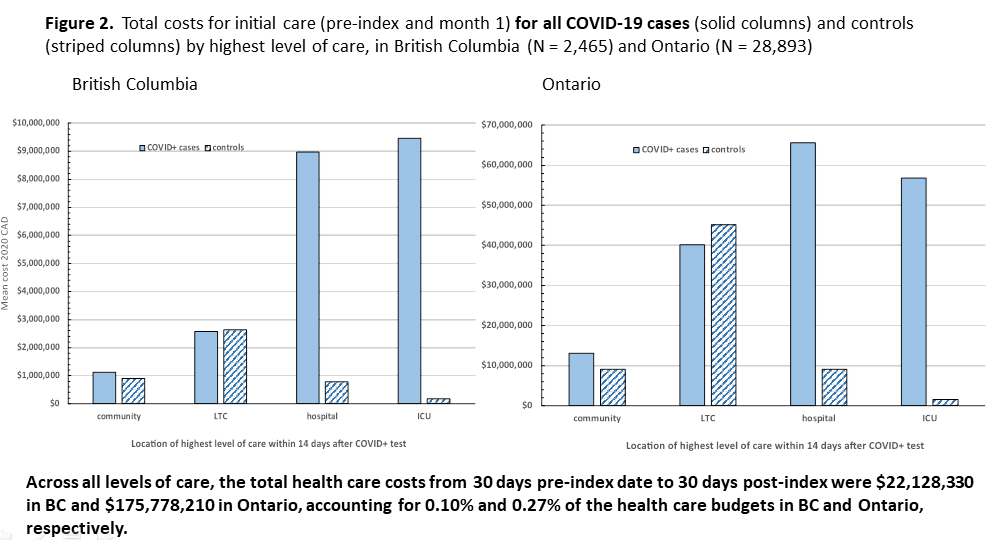
The research will measure how health system changes — including the cancellation or delaying of care — has impacted hospitalizations, physicians services, home care, long-term care, and other resources. The research team will study data from B.C. and Ontario that describe almost every interaction with the health system, providing a "population level" look at the health system.
“Looking at health systems as a whole will allow us to plan for system stresses related to COVID-19 resurgence and future pandemics, and ensure that we can meet the needs of Canadians even under conditions of health system strain,” said Krahn, who is based at UHN.

PUBLIC HEALTH AND UNIVERSITY-BASED INFORMATION
General Interest/Tracking Counts
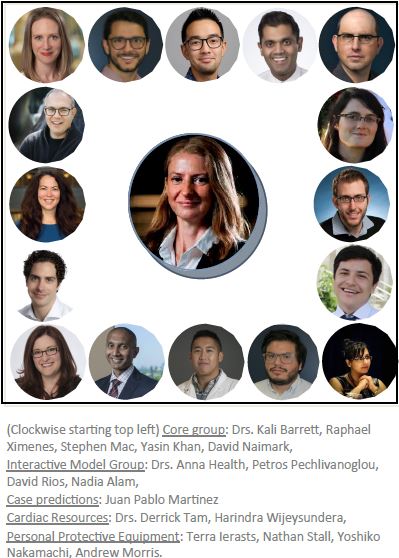
Mod Collab Group, Lead: Dr. Beate Sander
Our resident Canada Research Chair in Economics of Infectious Diseases, Dr. Beate Sander, has certainly been actively engaged in research throughout this pandemic, coordinating resource modeling in Ontario through the efforts of the COVID-19 Mod Collab group whose work will be used to inform public health policy in the province in tandem with Public Health Ontario and Ontario Health.
Using the CORE (COVID-19 Resource Estimator) Model 1.3, the team has modeled the burden on Ontario by forecasting the demand for ICU beds, ward beds, ventilators and personal protective equipment (PPE) bundles.
Method: The team’s model factored in a number of parameters including the number of COVID positive patients requiring hospitalization, taking into account whether or not the patient would need a ward or ICU bed, the number of ICU patients requiring a ventilator, the lengths of stay for a patent admitted to a ward or the ICU or both, and the probability of death (PoD) for patients who have to wait for an ICU bed or ventilator, as well as PoD for patients admitted to the ICU or ones with access to a ventilator. The team then modeled best, expected and worst case scenarios based on local data and those from other jurisdictions to help pinpoint when resource capacity may be reached.
Takeaways: The general tone of the expert advice offered by the group certainly emphasized the need to continue physical distancing as well as vastly increasing capacity for testing and contact tracing.
Emerging Research: the focus will be on group settings such as Long-Term Care (LTC) facilities, group homes and shelters. These facilities are currently facing exacerbated issues in dealing with COVID-19 partially due to less stringent protocols in LTCs vs. acute care hospitals, staffing shortages, and an even higher than normal requirement for PPE. LTC facilities are reportedly the new ’hotbed’ for COVID-19 cases.
The cardiac resources group is currently investigating the impact of the delays in patients undergoing cardiac procedures that were previously postponed due to COVID concerns, with waitlists rapidly growing.
All reports are available at the team's site. Updates can be found here: https://www.covid-19-mc.ca/home.
External Modelling Links
Shared Decision Making for Surgical Care in the Era of COVID-19.
Forner D, Noel CW, Densmore R, Goldstein DP, Corsten M, Pieterse AH, Shuman AG, Hong P, Rac VE. Otolaryngol Head Neck Surg. 2020 Sep 1:194599820954138. doi: 10.1177/0194599820954138. Epub ahead of print. PMID: 32867581.